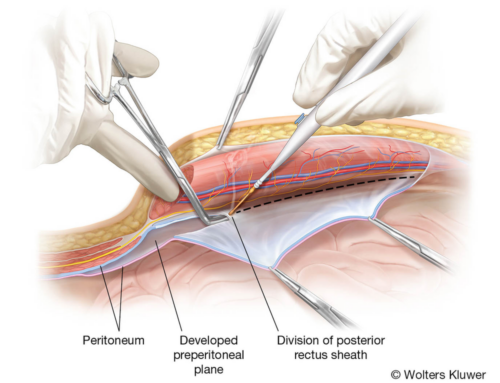
We always use modern and up-to-date scientific sources in our work. Our scientific advisor did a lot of research work to come up with relevant information for the creation of this medical animation about vaginal biofilm.
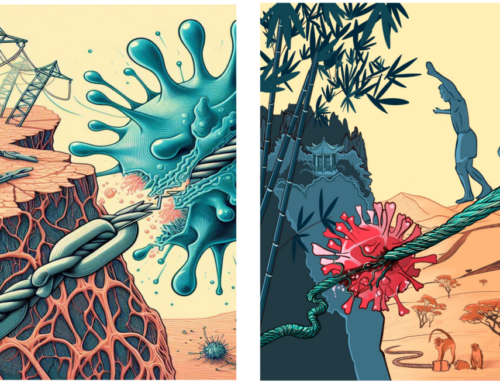
What is bacterial biofilm
A bacterial biofilm is a structured community of bacteria that is adherent to an inert surface or biological tissue. The biofilm is enclosed in a mucous substance: a self-produced matrix of extracellular polymeric substances (EPS). This community is often characterized by a complex internal architecture and contains channels allowing circulation of nutrients. Separate areas in the biofilm can contain genetically identical cells that exhibit different patterns of gene expression. This results in enhanced tolerance to adverse conditions and better persistence in hostile environments. It offers protection against chemical disinfection, antimicrobial treatment, and human immune responses.
Bacterial biofilm infections
Biofilm infections share clinical characteristics, regardless of in site in the human body where the biofilm develops. Biofilms grow slowly, and symptoms usually appear gradually. Biofilm communities are rarely entirely eradicated by the host defense mechanisms. Sessile bacterial biofilm cells release antigens resulting in increased antibody production. However, due to the biofilm structure, the produced antibodies are not capable of killing the biofilm bacteria and accumulate in the surrounding tissues. This can result in immune complex-related damage to the same tissues. The biofilm also attracts neutrophils that continuously release antimicrobial granule contents and reactive oxygen species that promote collagen degradation and subsequent host tissue injury.
On top of that, as antibiotic therapy fails to eradicate all bacteria in the biofilm, only the symptoms caused by the dispersed biofilm bacteria are reversed after treatment. As a result, even after multiple cycles of antibiotic therapy, biofilm infections are characterized by relapses of the condition. In summary, bacterial biofilm causes persistent, slowly progressing and chronic infections.
Increased antibiotic resistance and tolerance of biofilm cells
Decreased susceptibility to antimicrobial agents characterizes biofilms. Next, to the known mechanisms of bacterial resistance, treatment of biofilm-related illness is challenging due to the specific architecture of this biofilm. First of all, the applied antibiotics can be pumped out of the biofilm or can be degraded by the active bacteria in the outer biofilm subpopulation. Furthermore, the biofilm matrix forms a barrier against all antibiotics, even though this is not entirely impermeable (as demonstrated by mathematical models and experimentally for some antibiotics). Relatively large antibiotic compounds may be constrained by the viscous matrix and be slowed down, resulting in decreased penetration in the biofilm. The matrix components can also chemically neutralize antimicrobial compounds. Other biofilm environment-related factors, such as differences in pH, pCO2 or pO2, may further affect the efficacy of the antimicrobials. Due to the existence of several bacteria layers in the biofilm, nutrients and oxygen are depleted in the biofilm core. This nutrition and oxygen gradient slows down the growth and metabolism of bacteria in the inner stratum of the biofilm. The subpopulation of bacteria residing in the biofilm core is a group of dormant bacteria, and the biofilm growth conditions can influence their presence. When exposed to antibiotics, some of the dormant bacteria acquire increased tolerance towards antibiotics without undergoing genetic changes and are known as ‘persisters.’ In 1942, Hobby et al. discovered that 1% of Staphylococcus aureus cells were not killed by penicillin. As such, persister cells can lead to relapses after treatment: when the concentration of antibiotic compounds drops, the persister cells revert to their phenotype, causing re-growth of the biofilm.
Biofilm-associated with bacterial vaginosis (BV)
A healthy vaginal microbiome can be defined as a vaginal environment in which infections or symptoms are absent, and that is associated with a good reproductive health outcome. Furthermore, the healthy vaginal microbiome is typically dominated by a limited number of different Lactobacillus species, whereas BV is a polymicrobial dysbiosis. The lactobacilli concentration (except Lactobacillus iners) decreases during BV, while the bacterial load of other (facultative) anaerobic bacteria, such as Gardnerella vaginalis, Atopobium vaginae, Prevotella spp., Sneathia spp. and many others increase.
Biofilm in bacterial vaginosis
The ability of G. vaginalis, probably the most prevalent and abundant species in BV, to colonize human cells was already established in the eighties. The presence of epithelial cells covered with bacteria, or clue cells (meaning: characteristic cells that provide a clue to recognizing BV), is one of the Amsel criteria used in clinical settings to diagnose the condition. Such coating of epithelial cells with multiple layers of bacteria is exactly what one expects to see in case of biofilm formation. In reality, we have been looking at clue cells for decades, without realizing that we were dealing with biofilm formation. However, it was not until 2005 that Swidsinski and colleagues demonstrated the presence of this polymicrobial biofilm adhering to the vaginal epithelial cells in BV, using fluorescence in situ hybridization (FISH). After this first demonstration, other groups developed probes for other associated bacteria to visualize microorganisms involved in BV. Providing further evidence for the biofilm nature of BV, the treatment of BV is very challenging due to recurrence and relapses after antibiotic therapy, as is also the case in other biofilm-associated infections. Little is known about the exact mechanisms of biofilm formation in BV: the genes responsible, communication strategies (quorum sensing, metabolic communication) and genetic exchanges between biofilm-associated bacteria. Although it has been established that BV is a polymicrobial condition that involves a polymicrobial biofilm, we do not know the importance of the separate members nor the mechanisms of how these species interact. As such, it is not clear whether all species found in the BV biofilm have a role in pathogenesis, or are simply a consequence of biofilm formation on the vaginal epithelium. Lactobacillus-dominated vaginal microbiome. The availability of glycogen supports the health-associated vaginal microbiome that acts as a carbon source for Lactobacillus species that maintain the low vaginal pH which exerts selective antimicrobial activity. Lactobacilli also produce bacteriocins and compete for receptor sites on the vaginal epithelium with non-advantageous and pathogenic species. Limited in vitro data reveal synergistic interactions between G. vaginalis and other BV-associated bacteria. G. vaginalis is thought to be an essential player in BV, even though it also occurs in the healthy vaginal microbiome. However, genomic and microbiological data suggest the existence of multiple lineages of G. vaginalis, among which presumably not all strains will be able to cause BV. The presence of G. vaginalis in vaginal eubiosis as well as in vaginal dysbiosis might be the result of a mere quantitative difference, with many more cells of this species present in dysbiosis, but qualitative differences might be evoked as well. A possible explanation for this phenomenon may be related to a lower capacity of initial adhesion to the vaginal epithelium of a specific subset of G. vaginalis strains. G. vaginalis has multiple virulence factors that may contribute to the development of a biofilm. Specifically, the presence of fimbriae and the ability to produce sialidase, and vaginolysin could play a significant role in the colonization of the vaginal epithelial cells, and its ability to produce EPS could be important in the maturation of the biofilm. It is therefore tempting to consider G. vaginalis as the initial colonizer that provides a scaffold to which other bacteria, secondary colonizers, attach to establish a mature biofilm. One of these secondary colonizers is A. vaginae, an obligate anaerobic species, that has been linked to BV, and that, unlike G. vaginalis, is usually not present in the health-related vaginal microbiome. The detection of a vaginal biofilm with both G. vaginalis and A. vaginae is associated with a higher probability of having BV, as assessed by the Nugent criteria.
References:
The post Bacterial biofilm in the vagina appeared first on Nanobot Medical Animation Studio.