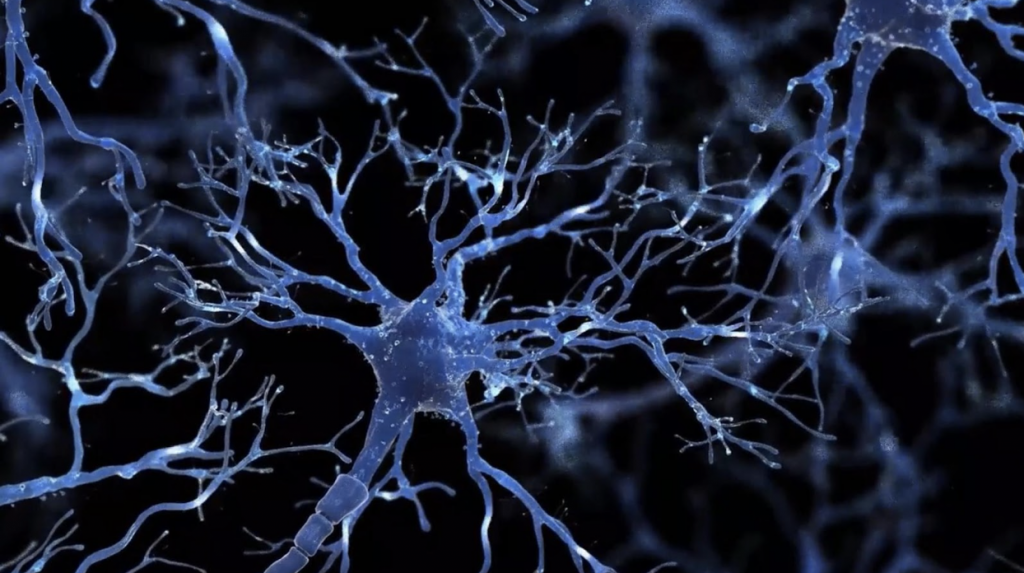
Worldwide, more than 50 million people are affected by neurodegenerative diseases, and Alzheimer’s disease is considered the most frequent type of neurodegenerative disease, occurring in 60% to 80% of all cases. Alzheimer’s pathology results from damage in the central nervous system, including abnormal aggregation of proteins in the nervous system and neurodegenerative processes. Amyloid plaques composed of beta-amyloid peptides (Aβ) have been identified in Alzheimer’s disease, which accumulates abnormally outside the nerve cells, and neurofibrillary tangles due to the hyper-phosphorylated tau protein, which accumulates in neurons. During the past decade, research efforts have focused on soluble Aβ oligomers, which are a more toxic and disease-relevant form of Aβ.

Current drug treatments for Alzheimer’s disease are symptomatic-based rather than curative to limit the progression of symptoms of dementia. Four drugs (donepezil, memantine, galantamine, rivastigmine) are approved on the market and belong to two families: anticholinesterase inhibitors and anti-glutaminergics. These drug treatments are used to delay the evolution of the disease.
Immunotherapies using antibodies to reduce assembled Aβ provide a promising approach and have been widely investigated since 1999. At least two factors are causing the inconsistent results with antibody drugs against Aβ: the limited brain penetration and lack of selectivity for the soluble Aβ oligomers.
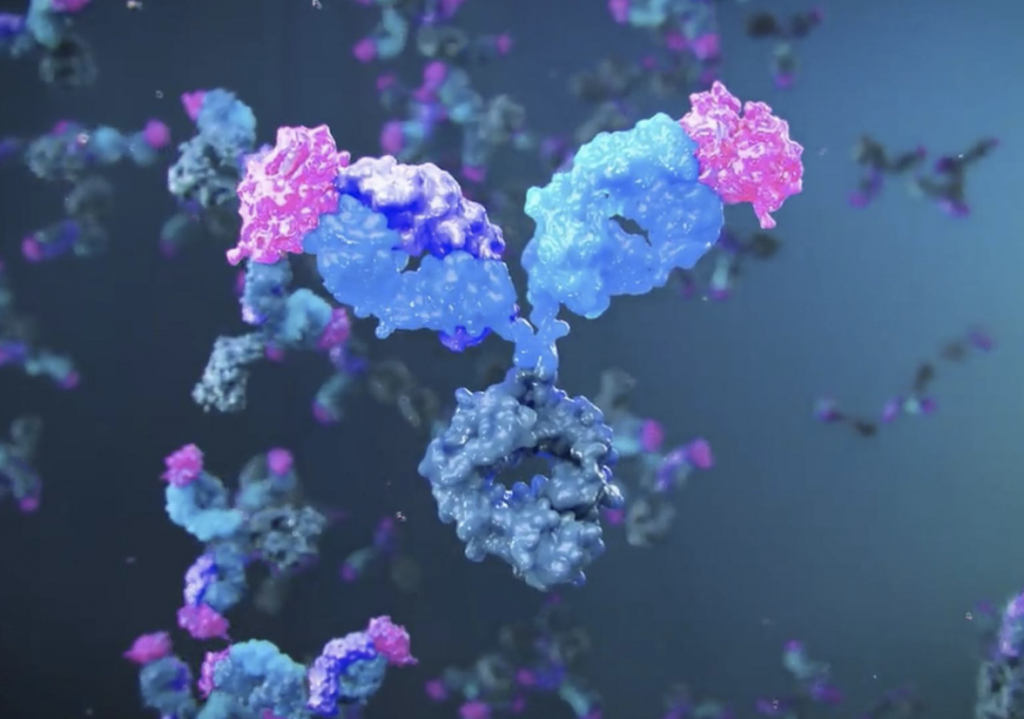
Roche investigated monoclonal antibodies crenezumab and gantenerumab that unfortunately last year showed unpromising results in clinical studies. Crenezumab specifically recognizes Aβ peptides and clears excess Aβ while exerting reduced subsequent effector function on microglia; the rationale was to stimulate amyloid phagocytosis while limiting the release of inflammatory cytokines as a way to avoid side effects such as vasogenic edema. According to a recent update to the phase 2 Alzheimer’s Prevention Initiative Autosomal Dominant Alzheimer’s Disease Colombia trial, crenezumab did not demonstrate a statistically significant benefit in either of its co-primary endpoints assessing the rate of change in cognitive abilities or episodic memory function in cognitively unimpaired persons at risk for Alzheimer disease.
In November, Roche announced results from the Phase III GRADUATE studies gantenerumab, an investigational anti-amyloid beta antibody, designed to bind with subnanomolar affinity to a conformational epitope on Aβ fibrils in people with early Alzheimer’s disease. The company reported that the studies did not meet their primary endpoint of slowing clinical decline on the global cognitive and functional scale, CDR-SB, at 116 weeks. Participants receiving gantenerumab showed a relative reduction in the clinical decline of 8% and 6% studies compared with placebo, however, those results were not statistically significant.
Donanemab, another antibody that targets a modified form of deposited Aβ, is being investigated for the treatment of early Alzheimer’s disease.
Eli Lilly and Company has announced that donanemab met all primary and secondary endpoints for the 6-month primary outcome analysis in the Phase 3 TRAILBLAZER-ALZ 4 study, providing the first active comparator data on amyloid plaque clearance in patients with early symptomatic Alzheimer’s disease treated with amyloid-targeting therapies. Brain amyloid clearance was achieved in 37.9% of donanemab-treated participants compared with 1.6% of Aduhelm-treated patients at 6 months. Donanemab reduced brain amyloid plaque levels vs. baseline by 65.2% compared with 17.0% for Aduhelm at 6 months.
Recently, The FDA granted approval for the Alzheimer’s drug lecanemab the treatment from Biogen and Eisai. Lecanemab is a monoclonal antibody that binds with high affinity to Aβ soluble protofibrils. The FDA’s approval comes after clinical trial results published in November indicated that lecanemab slows cognitive decline somewhat in people with mild impairment due to Alzheimer’s disease, but the treatment also carries risks of brain swelling and bleeding.
The development of disease-modifying therapies for Alzheimer’s disease is an urgent issue. Progress in the understanding of pathophysiology based on the amyloid hypothesis has led to the development of numerous candidate disease-modifying therapies over the past years. There is a hope that disease-modifying therapies against Alzheimer’s disease will be presented very soon.
The post Alzheimer’s disease: promising and failed investigational drugs appeared first on Nanobot.